LUNG INVOLVEMENT IN RHEUMATOLOGIC DISEASES

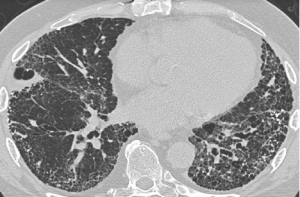
Lung involvement in autoimmune rheumatic diseases is a common manifestation and a major cause of mortality and morbidity. Involvement may include lung parenchyma, airways, pleura, vessels and respiratory muscles. Main differential diagnoses include rheumatic disease manifestation, drug-induced manifestation or infection.
Interstitial lung disease (ILD) in connective tissue disease (CTD) can be characterized using the classification of the idiopathic interstitial pneumonias. CTDs as a whole may develop all histologic patterns observed in idiopathic interstitial pneumonias. Systemic sclerosis is most frequently associated with ILD and, in most of these patients, ILD manifests as a histological pattern of nonspecific interstitial pneumonia. Conversely, in rheumatoid arthritis, the pattern of ILD seems to be most often usual interstitial pneumonia. Histologic patterns may be combined, as exemplified by the frequent association of ILD with lymphocytic bronchiolitis in rheumatoid arthritis. Occasionally, lung involvement can present before the diagnosis of CTD, especially in idiopathic inflammatory myopathy and rheumatoid arthritis.
Symptoms
• Breathlessness
• Cough
• Cyanosis
• Chest pain
• Hemoptysis/Blood in sputum
• Respiratory failure
• Fever
• Weight loss
Treatment
• Immunosuppressive drugs including glucocorticoids
• Antifibrotic drugs
• Management of PAH (Pulmonary Artery Hypertension)
• Oxygen therapy, continuous or intermittent
The key goals of the clinical assessment of patients with both ILD and CTD are the detection of ILD and prognostic evaluation to determine which patients should be treated and how.


